
We’re going to Crufts Hall 3 Stand 14. March 5–8, 2026

We’re going to Crufts Hall 3 Stand 14. March 5–8, 2026
Patients will not determine their own pessary size. If a pessary is considered an appropriate treatment for vaginal prolapse, a clinician—such as a doctor, nurse, or gynecologist—will make this decision. Using an internal examination, they will select the appropriate material, shape, and size from the available options to ensure the best fit and effectiveness.
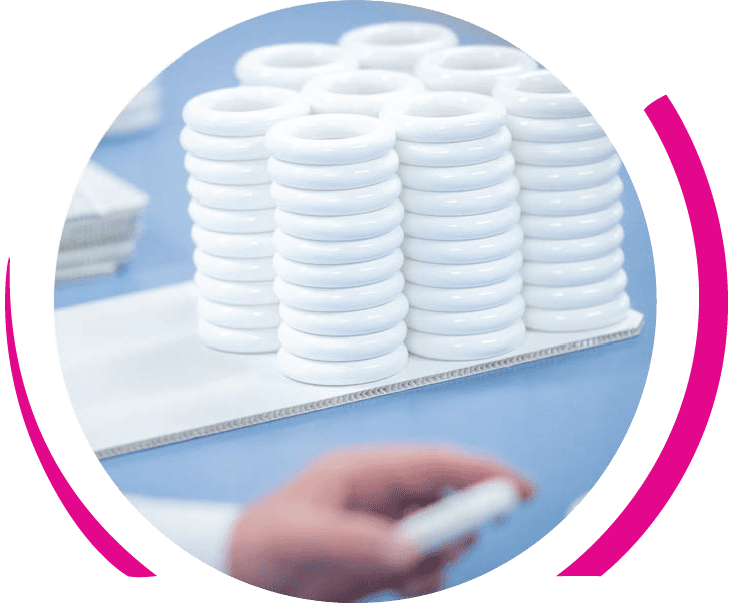
Ring pessaries are non-invasive devices that support pelvic organs, alleviating symptoms of pelvic organ prolapse and stress incontinence.
Correct sizing of pessaries is crucial for comfort and effectiveness, with variations in size significantly affecting fit and performance.
Regular follow-up care is essential to monitor the pessary’s fit and condition, preventing complications and ensuring long-term effectiveness.
Selecting the correct pessary size is critical for ensuring comfort, effectiveness, and preventing complications. The process of determining the appropriate size involves placing a finger between the pessary and the vaginal wall and ensuring that the prolapse is reduced above the hymen. This method helps to ascertain that the pessary fits snugly without causing discomfort or dysuria.
A successful pessary fitting should retain the device during activities such as coughing, walking, or performing a Valsalva maneuver. If the pessary is not the right size, patients might experience discomfort or even expulsion of the device, which can compromise its effectiveness and lead to pessary failure.
Correct sizing ensures the device provides the necessary support without causing additional issues, thereby enhancing the user’s overall quality of life with the correct size.
The ring pessary size chart is vital for pessary fitting, with dimensions typically ranging from 50 mm to 100 mm in 5 mm increments to accommodate different anatomical needs. Clinicians use Pessary Ring Sizing Kits categorized into Small (50/55/60/65 mm), Medium (65/70/75/80 mm), and Large (85/90/95/100 mm) to help identify the most appropriate size pessary through pessary sizing.
Bray Healthcare offers a variety of pessary rings, including sizes such as 50mm, 53mm, 56mm, and so on, up to 100mm. Additionally, clinicians select from two ranges of ring pessaries designed to suit varying support needs. Choosing the appropriate size is crucial for proper positioning, allowing the pessary to sit snugly against the vaginal wall and perform its function effectively.
Correct use of the size chart by healthcare providers ensures the pessary fits well and provides the necessary support to alleviate symptoms of pelvic organ prolapse and stress incontinence.
Effectively using the ring pessary size chart involves:
Measuring vaginal width and length.
Consulting the size chart to find the appropriate size.
Selecting a pessary that adequately fills the vaginal space without causing pain or pressure.
When inserting a ring pessary, it should be positioned vertically before being released into a horizontal position within the vagina. This positioning helps create a suction seal that maintains the pessary’s position and prevents it from slipping or being expelled.
Following these steps and using the size chart correctly ensures the pessary fits well, providing the necessary support and comfort.
Measuring vaginal width is crucial for selecting the right pessary size, as variations can significantly affect the fit. During a vaginal examination, the width is typically measured using the index finger, single finger, and examining finger, gauging the distance from the posterior fornix to the pubic symphysis and the cervix.
Measurements are taken horizontally at the level of the cervix or vaginal vault to determine the appropriate pessary size, ensuring a snug fit that provides necessary support without causing discomfort.
Accurate measurements are vital in the pessary fitting process, ensuring the device is both effective and comfortable.
Ring pessaries are available in several sizes, with size 3, 4, and 5 being the most commonly used by women. These sizes are particularly effective in managing symptoms of pelvic organ prolapse (Stage I or II) and stress incontinence.
A correctly sized pessary should alleviate symptoms without being felt by the patient. Women often find ring pessaries easier to remove and insert compared to other types, making them a popular choice for self-management.
Knowing the common sizes and their uses helps in selecting the most appropriate pessary for individual needs, ensuring both comfort and effectiveness.
The trial and adjustment process for pessary fitting is essential for achieving the best results. Patient comfort and symptom relief are the primary goals of this process. It often involves trying multiple sizes before finding one that fits comfortably and securely.
If a pessary causes discomfort or is easily expelled, consider the following:
• Alternative sizes or types should be considered.
• Follow-up appointments are important.
• An initial evaluation should be scheduled after a week to assess the fit.
• Up to 46% of patients may require a re-fitting within the first week of use.
The trial and adjustment process is a common approach in pessary fitting, ensuring that the device provides maximum comfort and support.
Several contraindications and potential complications are associated with ring pessaries. Contraindications include infections such as vaginitis, latex sensitivity, and patient non-compliance. Other issues can involve fitting discomfort, bleeding, ulceration, and inflammation of the pelvic region.
Complications from using a pessary may include:
Discomfort
Abnormal vaginal bleeding
Vaginal discharge
Erosions
In severe cases, complications such as rectovaginal and vesicovaginal fistulas can occur, requiring surgery.
Understanding these contraindications and complications is crucial for safe and effective pessary use.
Regular follow-up appointments are crucial for monitoring the fit and condition of the pessary to ensure comfort and effectiveness. The recommended follow-up schedule is:
Return for a follow-up appointment within two weeks initially.
For non-self-managing patients, have regular checks every three months.
For self-managing patients, have regular checks every six months or annually.
During follow-up visits, assessments are made for symptoms such as pelvic floor pressure and urinary symptoms, and the vaginal tissues are inspected to ensure there are no complications related to prolapse and urinary symptoms. Patient compliance with follow-up appointments is critical, as a lack of compliance can lead to complications and dissatisfaction, impacting the overall treatment experience. The British Society of Urogynaecology emphasizes the importance of these evaluations.
Follow-up care is a vital component of managing pelvic organ prolapse with a ring pessary, ensuring long-term success and patient satisfaction in cases of advanced pelvic organ prolapse.
Proper fitting and sizing of ring pessaries are crucial for comfort and effectiveness in managing pelvic organ prolapse and stress incontinence. By understanding the importance of correct sizing, using the size chart effectively, and following the trial and adjustment process, patients can achieve the best results.
Encouraging self-management and regular follow-up care further enhance the overall experience, ensuring long-term success and patient satisfaction. With the right knowledge and approach, ring pessaries can significantly improve the quality of life for those affected by pelvic organ prolapse.
The most common sizes of ring pessaries used by women are 3, 4, and 5, which effectively manage pelvic organ prolapse and stress incontinence symptoms.
The correct size of a pessary is determined by placing a finger between the pessary and the vaginal wall, ensuring that there is adequate space and that prolapse is effectively reduced above the hymen. This method ensures proper fit and function.
Using a ring pessary may lead to complications such as discomfort, abnormal vaginal bleeding, vaginal discharge, and erosions. In severe cases, it could result in rectovaginal and vesicovaginal fistulas.
You cannot self-manage a Bray pessary. It must be managed and maintained by a doctor, nurse, or gynecologist.
Regular follow-up appointments are crucial for pessary users to monitor the fit and condition of the pessary, ensuring comfort and effectiveness while preventing potential complications.